Methods
Based on clinical observations and a series of pilot studies, we tested the following hypotheses:
1) The Pressure Pain Sensitivity measurement of the chest bone (PPS) measures stress and can distinguish between transient and persistent stress, as the latter is associated with autonomic nervous system dysfunction, measured as an elevated PPS at rest.
2) PPS measures the function of the autonomic nervous system in the brain, and an elevated resting PPS reflects autonomic dysfunction, mainly as sympathetic autonomic hyperactivity, and is most probably controlled by a non-beta-adrenergic receptor system.
3) Reduction of an elevated PPS is associated with a reduction of persistent stress and autonomic dysfunction.
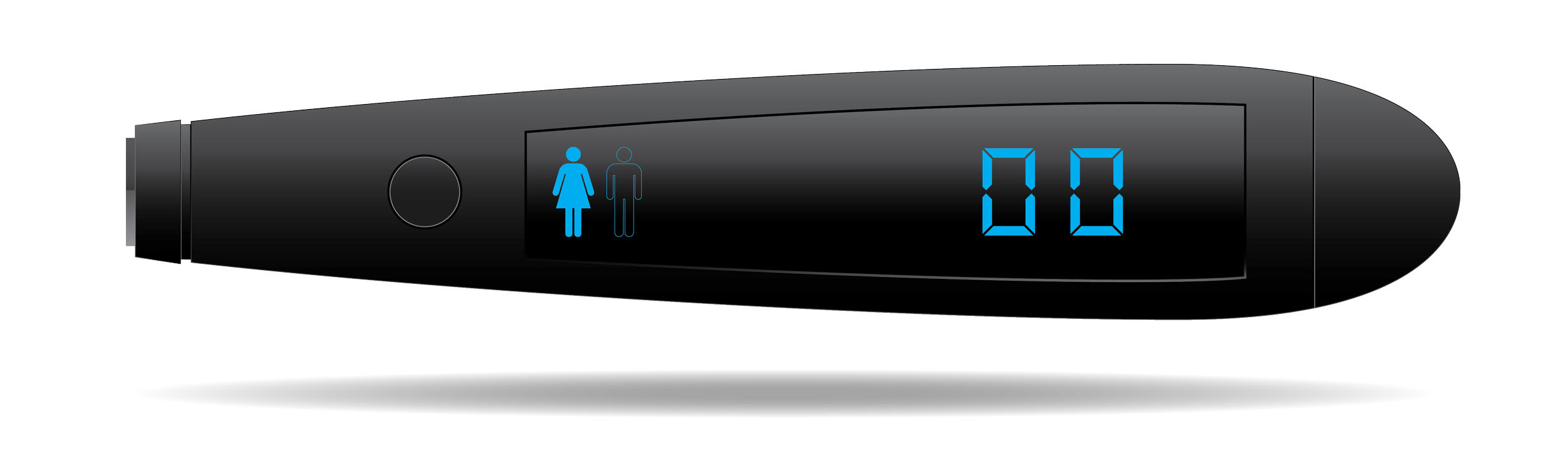
4) A specific non-pharmacological intervention can reduce an elevated resting PPS. This intervention is home-based and focuses on daily PPS measurements as a feedback measurement for behavioral guidance, daily non-noxious sensory nerve stimulation for PPS reduction, and ongoing professional surveillance for proactive action if PPS measurements are missing or deviating.
The hypotheses are currently tested in a combination of prospective experimental, cross-sectional, and randomized controlled interventional trials with top performers, healthy working people, people with type 2 diabetes, and people with stable ischemic heart disease.
Results
In healthy office workers, heart disease patients, and type 2 diabetes patients, it was found that PPS was associated with a broad range of questionnaire-related measurements of stress as well as with a broad range of cardiovascular health risk factors controlled by the autonomic nervous system (e.g., depression, blood pressure, pulse rate, and serum cholesterol). In these populations, the used intervention was found to reduce an elevated PPS, which was associated with improvement of the mentioned health risk factors. Beta-blockade medication had no effect on PPS, but inhibited the effect of reducing PPS on depression, work of the heart, blood pressure, and heart rate variability. In heart disease patients a meta-analysis showed a mortality rate substantially significant and 57% lower than that of the general population. In type 2 diabetes patients the reduction of dysregulated glycated hemoglobin was reduced by 22%. These effects were obtained with no risk of side effects or complications.