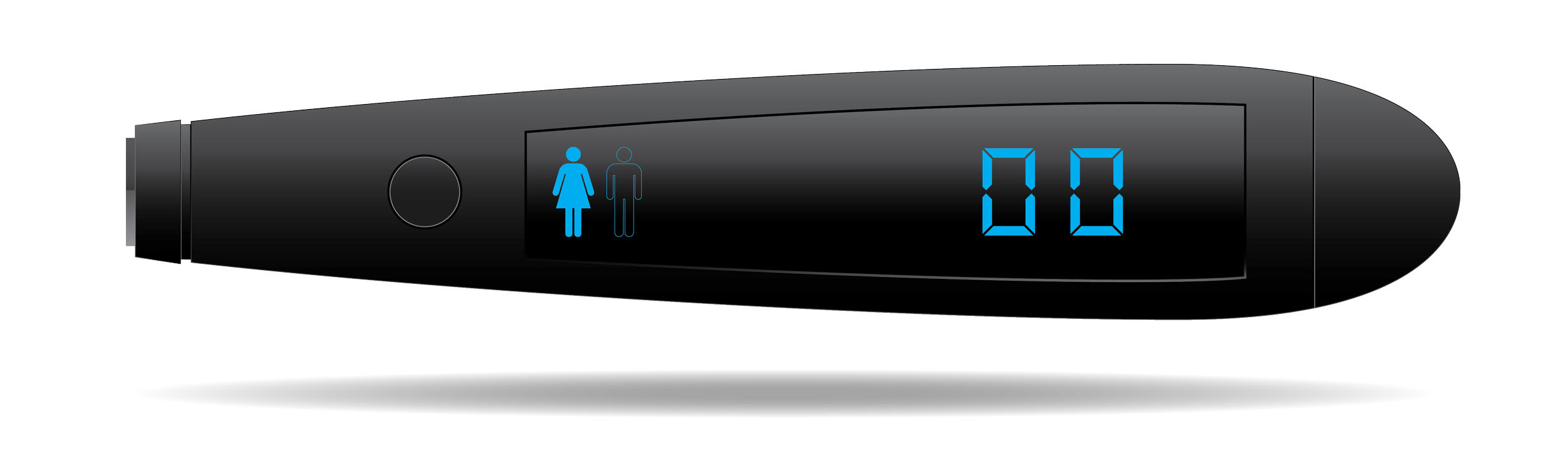
Figure 11. The association between mean change in PPS during tilt-table testing (∆ PPS Tilt test) and number of autonomic nervous system dysfunction (ANSD) risk factors, including chest pain at rest, hypertension (systolic blood pressure ≥ 130), depression (Major Depression Inventory score ≥ 20), and elevated level of persistent stress (resting PPS ≥ 60 units) (r = – 0.21, p < 0.0001; N = 361). The horizontal lines indicate 95% confidence intervals (Ballegaard et al 2015).
In a cross-sectional study on 111 persons with type 2 diabetes, an association between PPS and cardiovascular autonomic neuropathy was found as measured by a specific laboratory test for autonomic function (Vagus ®), including three tests: standing up, deep breathing, and Valsalva. PPS was closely associated to the standing up test but not to deep breathing and Valsalva, indicating that PPS is associated to sympathetic autonomic nervous activity (Faber et al 2021).
It is worth noting that among 308 Danish office workers, 27 % had an elevated PPS measurement (i.e., ≥ 60 arbitrary units) (Ballegaard et al 2012), while among 361 patients with chronic diseases such as stable ischemic heart disease, 59 % had an elevated PPS (Bergmann et al 2013), and more than 90 % of persons with type 2 diabetes from general practicesm which were screened for participation in a randomized controlled trial, had an elevated PPS while 55 % of persons with type 2 diabetes in hospital ambulatory setting had an elevated PPS (Faber et al 2021) .
Prospective randomized intervention studies
Among office workers with an elevated PPS, and when compared to a control group, the active group receiving the PPS-guided intervention obtained a clinically relevant reduction in PPS, blood pressure, heart rate, work of the heart, and serum cholesterol (Ballegaard et al 2014; Ballegaard 2017). Furthermore, the changes in PPS during the intervention period were found the be associated with these outcome measures, as well to body mass index, visceral fat index, glycated hemoglobin HbA1c, and the inflammatory marker YKL-40.
Among patients with stable ischemic heart disease, and when compared to a control group, the active group receiving the PPS-guided intervention obtained a reduction in depression symptoms, improvement of wellbeing (Bergmann et al 2014), restoration of autonomic dysfunction measured by tilt table testing, and reduction of number of autonomic nervous system dysfunction risk factors (Ballegaard et al 2015). Furthermore, among the most vulnerable patients with overt depression, the Cohen effect size with respect to anti-depressive effect was 0.9, which is substantially higher than the 0.3 effect size obtained by anti-depressive medication (Ballegaard 2017).
Beta-blockade medication inhibits the efferent sympathetic autonomic activity. When the group of patients receiving beta-blockade medication was compared to the non-user group, an inhibiting effect was observed with respect to the anti-depressive effect and the increase in blood pressure response to a tilt table test. However, the reduction in PPS and the increase in PPS response to a tilt table test during the intervention period, was not significantly influenced by the beta-blockade medication (Ballegaard et al 2016).
The effect of beta-blockade medication has also been studied in 111 persons with type 2 diabetes. It was found that PPS was unaffected, but heart rate was lower in persons with beta-blockade medication (Faber et al 2021).
In a randomized prospective intervention study in patients with stable ischemic heart disease, using the response to a tilt table test as a fully controllable experimental stimulation of autonomic nervous system function, the responses of PPS and heart rate variability (HRV) were compared to those of blood pressure, heart rate, and work of the heart measured as systolic blood pressure x heart rate (the Double Product). The association between PPS and the cardiovascular response to tilting was close. It was also present for HRV, but significantly less prominent than for PPS. In addition, the effect of 3 months of use of the PPS guided intervention with the aim to reduce an elevated PPS measurement was studied. This study showed that when resting PPS decreases during intervention, the response in PPS to tilting increases, and this increase was closely associated to a similar increase in systolic blood pressure and heart rate response to tilting (publication in preparation).
In a randomized prospective intervention study, PPS was included as an outcome measurement for the effect of a physical exercise rehabilitation program in patients with minor stroke. The study demonstrates that exercise rehabilitation (e.g., two hours of vigorous exercise per week) in minor stroke patients does not change oxygen uptake, muscle strength, quality of life, and in line with this the PPS measurement does not change (Krawcyk R et al 2019).
In an experimental cross-over study on healthy opera students, it was found that work of the heart (i.e., the Double Product) and PPS were strongly associated in response to experimental short duration physical exercise. During two minutes of physical exercise the Double Product increased and PPS decreased, while this was reversed in the two minute post-exercise recovery resting period; that is the Double Product decreased and PPS increased (Ballegaard et al 2009).
Taken together these two studies may indicate that short-term physical exercise has a pronounced reducing effect on PPS. However, in the case of autonomic dysfunction and thus reduced resilience, there is no lasting effect on an elevated PPS when the physical exercise is conducted only 4 times a week. Future studies may elucidate if more frequently conducted short-term physical exercise may have the potential to reduce an elevated PPS as a sign of autonomic dysfunction.
In a randomized controlled trial including 144 persons with type 2 diabetes, it was found that PPS and glycated hemoglobin (hbA1c) as a measurement for cerebral glucose metabolism were closely related, and that a non-pharmacological reduction of an elevated PPS was associated with a reduction of HbA1c (Faber et al 2021). Furthermore, it was found that PPS was closely related to the cerebral regulation of glycated hemoglobin, measured as a close correlation between baseline HbA1c and the reduction of HbA1c, when an elevated PPS was reduced; that is the higher the baseline HbA1c the larger the reduction of HbA1c, when the group of persons who achieved a reduction in PPS and when compared to persons, who did not achieve a reduction in PPS (Faber et al 2023).
In a randomized prospective intervention study in patients with diabetes type 1, the PPS-guided intervention with the aim to reduce an elevated PPS — and thus treat autonomous nervous system dysfunction — was tested. This study demonstrated a robust reduction in PPS due to the intervention. The adherence to PPS measurement and treatment was high. Thus as an implementation study this was as success. This study was performed as part of a PhD thesis.
In a randomized trial of 213 persons with stable ischemic heart disease, the 5-year all-cause mortality was studied with the aim to explore previous findings in two prospective case-control studies (Ballegaard et al 2004; Magnusson et al 2010) of an effect on all-cause mortality from a non-pharmacological intervention which aimed at reducing an elevated PPS, but with the possibility of elimination the potential influence from selection bias and researcher bias. When compared to the general Danish population, matched for age, gender, and observation period, it was found that the active group had a significant 75% reduction in mortality, while the control group had a mortality like the general population. When comparing active and control group of the randomized trial, the reduction in the active group was significant and 81% (Faber et al 2023[abstract accepted). In a meta-analysis pooling data from the three consecutive studies who compared the effect on all-cause mortality of the non-pharmacological reduction of an elevated PPS in persons with manifest atherosclerotic cardiovascular disease with that of the general population, it was found that mean reduction in 4 years all-cause mortality was highly significant and 57%. It should be noted that persons with ischemic heart disease have an elevated mortality when compared to the general population. Furthermore, the effect from medication and invasive treatment in persons with stable ischemic disease are modest at best and, in contrast to the present intervention, they are associated with side effects and risks (Califf, DeMets 2002; Hochman et al 2022).